Confidence Interval Analysis Cia Software Download

Methods This retrospective cohort study involved 152 patients with ALI enrolled in the Fluid and Catheter Treatment Trial (FACTT) from five NHLBI ARDS (Acute Respiratory Distress Syndrome) Network sites. VPW and central venous pressure (CVP) or pulmonary artery occlusion pressure (PAOP) from the first four study days were correlated. The relationships between VPW, positive end-expiratory pressure (PEEP), cumulative fluid balance, and PAOP were also evaluated.
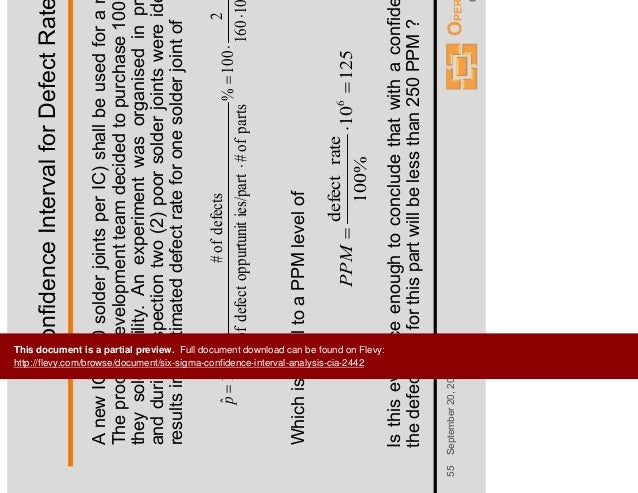
Significance testing was two sided at the 5% level. We used the software package SPIDA.13 Relative risk and confidence intervals were calculated with CIA software.14 The study was approved by the national ethics committee.
Receiver operator characteristic (ROC) curves were used to determine the ability of VPW to detect PAOP. Results A total of 71 and 152 patients provided 118 and 276 paired VPW/PAOP and VPW/CVP measurements, respectively. VPW correlated with PAOP (r = 0.41; P. The NIH NHLBI ARDS Network Fluid and Catheter Treatment Trial (FACTT) demonstrated that fluid management for patients with acute lung injury (ALI) using a protocol guided by intravascular pressure measurements from a central venous catheter (CVC) resulted in similar clinical outcomes compared to fluid management directed by measurements from a pulmonary artery catheter (PAC) [ ]. The PAC group experienced significantly more nonfatal complications, mostly in the form of arrhythmias.
These results, combined with previous studies demonstrating either lack of benefit or increased harm, have led many experts to discourage the routine use of the PAC in patients with ALI [, ]. Regardless of the type of catheter, a conservative fluid management strategy in ALI patients increased the number of days alive and free from mechanical ventilation [ ]. Central venous pressure (CVP) or pulmonary artery occlusion pressure (PAOP) was used to generate instructions and function as targets for the fluid management strategies in this trial.
It remains unknown if such invasive measurements are required for management of critically ill patients or if non-invasive measurements would suffice. Portable chest x-rays (CXR) are obtained frequently in patients with ALI.
In previous studies, the vascular pedicle width (VPW), either alone or in conjunction with the cardiothoracic ratio (CTR), which are both easily measured on most portable CXRs [ ], has correlated with intravascular volume status in both critically ill and non-critically ill patients [ – ]. Despite these data, monitoring of VPW is not part of standard practice. The purpose of this study was to investigate the relationship between non-invasive measures of intravascular volume status, namely the VPW and CTR and invasive intravascular pressure measurements, namely CVP and/or PAOP, in ALI patients enrolled in the FACTT study at five Acute Respiratory Distress Syndrome (ARDS) Network sites. In addition, the ability of VPW to discriminate when the edema had a hydrostatic component or when conservative fluid management goals were achieved was also investigated. Patients included in this analysis were a subset of patients enrolled in the ARDS Network Fluid and Catheter Treatment Trial (FACTT).
All centers enrolling in FACTT obtained local IRB approval and all patients or their surrogates provided informed consent. This data analysis was also specifically considered exempt by the Vanderbilt Institutional Review Board. FACTT was a multi-center, randomized clinical trial of two different fluid strategies (conservative vs.
Liberal) factorialized with two different methods of intravascular pressure measurement (CVP or PAOP). The patients randomized to receive PAC had both PAOP and CVP measurements while only CVP measurements were available for those randomized to management with a CVC.
Neither CVP nor PAOP measurements were adjusted for positive-end expiratory pressure (PEEP) levels. FACTT used a standardized fluid management protocol [ ], which attempted to achieve intravascular pressure targets when patients were not in shock and had adequate renal and circulatory function. Intravascular pressure measurements were taken every four hours for the shorter of seven days or duration of mechanical ventilation. Two intravascular measurements were recorded daily; one from 08:00 AM and a second from a random protocol check time which changed each day. Raskraska astana bajterek en. To be eligible for this substudy, patients enrolled in FACTT must have had both a chest radiograph available for review and a 'matching' intravascular pressure measurement for any day between study days 0 through 4. Matching intravascular pressure measurement was defined as a CVP and/or PAOP measurement obtained within three hours before or after the time of the chest radiograph.